Address: 21660 W Field Pkwy, Suite 301, Deer Park, IL 60010

Postpartum “Baby Blues” vs. Postpartum Depression
Understanding the Key Differences
10/7/2025


Bringing a baby into the world is one of the most profound emotional experiences a person can have. It’s filled with joy, love, and a deep sense of purpose — but for many new mothers, it can also bring unexpected feelings of sadness, anxiety, and exhaustion. These emotional changes are common and often misunderstood. While many women experience postpartum “baby blues”, some develop a more serious condition known as postpartum depression (PPD).
Understanding the difference between the two is critical for early intervention and healing — and today, new treatments such as ketamine infusion therapy are offering hope for faster, more effective relief.
What Are the “Baby Blues”?
After childbirth, your body goes through massive hormonal shifts. Estrogen and progesterone levels plummet dramatically, and these fluctuations can affect mood regulation. Combined with physical exhaustion, disrupted sleep, and the stress of caring for a newborn, many women experience emotional ups and downs. This is what’s commonly referred to as the “baby blues.”
Typical Characteristics of Baby Blues:
● Emotional sensitivity and frequent crying spells
● Mild anxiety or irritability
● Difficulty concentrating
● Trouble sleeping (even when the baby sleeps)
● Feeling overwhelmed but still able to care for your baby
These symptoms usually begin within the first few days after delivery and resolve on their own within two weeks. The key feature is that the mother can still find joy in her baby and daily activities, even though she feels tearful or moody.
Why Baby Blues Happen
Physiological and emotional transitions play a major role:
● Hormonal shifts after childbirth affect neurotransmitters such as serotonin and dopamine.
● Physical recovery from labor, pain, and sleep loss can heighten emotional vulnerability.
● Lifestyle changes — loss of routine, isolation, and new responsibilities — add stress.
Baby blues are normal and self-limiting. What matters most is recognizing when it’s not just baby blues anymore.
What Is Postpartum Depression?
Unlike the baby blues, postpartum depression (PPD) is a serious medical condition that affects approximately 1 in 7 new mothers, according to the American Psychological Association. It involves persistent, intense, and disabling mood symptoms that interfere with daily functioning and bonding with the baby.
Common Symptoms of Postpartum Depression
● Persistent sadness or hopelessness lasting more than two weeks
● Loss of interest or pleasure in activities (including caring for the baby)
● Fatigue, irritability, or agitation
● Feelings of worthlessness, guilt, or being an inadequate parent
● Significant anxiety or panic attacks
● Changes in appetite or sleep patterns
● Difficulty concentrating or making decisions
● Thoughts of harming oneself or the baby (in severe cases)
PPD typically develops within the first few weeks to months after delivery, but it can appear up to a year postpartum. Unlike baby blues, it does not resolve without treatment and can worsen over time if left unaddressed.
If symptoms last beyond two weeks or worsen in intensity, it’s time to seek professional help. Postpartum depression is not a sign of weakness — it’s a medical condition that can be effectively treated with proper care.
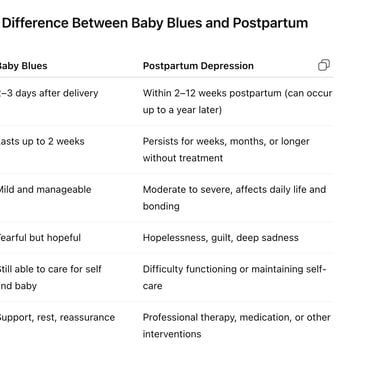
How to Tell the Difference Between Baby Blues and Postpartum Depression
Why It’s Important to Seek Help Early
Untreated postpartum depression can have lasting effects on both mother and baby:
● Mother’s health: Increased risk of chronic depression, anxiety, and suicidal thoughts.
● Infant’s development: Emotional unavailability of the parent can impact attachment, emotional regulation, and even cognitive development in the child.
● Family well-being: PPD can strain relationships and reduce the family’s ability to adapt to life changes.
The good news is that postpartum depression is highly treatable, and modern medicine is expanding the range of safe, effective therapies — including new approaches like ketamine infusion therapy.
Steps You Can Take if You Suspect Postpartum Depression
Ketamine Infusion Therapy: A Breakthrough for Postpartum Depression
Ketamine — once known mainly as an anesthetic — is now one of the most promising treatments for treatment-resistant depression, including postpartum depression. It works differently from traditional antidepressants, which can take weeks or months to show benefits.
How Ketamine Works
Ketamine acts on glutamate, one of the brain’s main neurotransmitters, rather than serotonin. By targeting NMDA (N-methyl-D-aspartate) receptors, it triggers a rapid increase in synaptic connections and neuroplasticity, allowing the brain to rewire itself toward a healthier mood regulation.
Benefits of Ketamine for Postpartum Depression
● Rapid relief: Some patients report improvement within hours to days, not weeks.
● Effective for resistant cases: Works even when traditional antidepressants fail.
● Improved motivation and bonding: Restores emotional engagement and energy.
● Low-dose and monitored: Administered safely under medical supervision, with minimal side effects.
Research has shown that ketamine can lift severe depressive symptoms — including suicidal thoughts — quickly, offering a lifeline to mothers in crisis.
Safety and Considerations
Ketamine infusion therapy should only be performed in licensed medical facilities by trained professionals experienced in mental health and anesthetic care. While generally well-tolerated, it may not be suitable for everyone, especially during breastfeeding. Each case requires individual evaluation by a clinician.
Other Treatment Options for Postpartum Depression
While ketamine is a powerful tool, it’s part of a broader continuum of care. The most effective treatment plans often combine multiple approaches:
1. Psychotherapy (Talk Therapy)
○ Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT) are highly effective.
○ Helps identify negative thought patterns and strengthen coping skills.
2. Medication
○ Antidepressants (such as SSRIs) may be prescribed when symptoms are moderate to severe.
○ Physicians carefully choose medications compatible with breastfeeding when necessary.
3. Lifestyle and Support Interventions
○ Sleep hygiene, balanced nutrition, gentle physical activity, and mindfulness can improve recovery.
○ Family education and peer support groups reduce isolation and stigma.
4. Hormone-Based Therapies
○ In some cases, restoring hormonal balance (for example, through brexanolone infusion or estrogen therapy) can relieve symptoms.
Each patient’s needs are unique — and an integrated approach offers the best outcomes.
If you or someone you love may be experiencing postpartum depression:
1. Acknowledge your feelings — they are valid and not your fault.
2. Seek professional help early. Talk to your OB-GYN, primary care provider, or a mental health specialist.
3. Build your support system. Confide in trusted family or friends.
4. Ask about new treatment options. If conventional therapies haven’t helped, inquire about ketamine infusion or other advanced treatments.
5. Prioritize rest and nutrition. Self-care is not selfish — it’s essential for healing.
Remember: postpartum depression is not a personal failure. It’s a treatable medical condition, and with the right help, recovery is absolutely possible.
The Bottom Line
Postpartum “baby blues” and postpartum depression share some emotional overlap, but they differ in intensity, duration, and impact. Baby blues are short-lived and mild, while postpartum depression is deeper, more persistent, and requires professional treatment.
With the advancement of modern therapies — especially ketamine infusion therapy — there’s new hope for mothers who haven’t found relief with traditional medications. Fast, effective, and safe under clinical supervision, ketamine is helping transform postpartum care and saving lives.
If you or someone you know is struggling after childbirth, reach out for help today. Healing starts with a conversation — and you are never alone.

Health Care Professionals' Resources
Sign Up To Receive The Latest Updates On Ketamine Infusion Therapy And Spravato Nasal Spray For Mental Health




Contact Us
21660 W Field Pkwy
Suite 301
Deer Park, IL 60010
Phone:
847-232-4045
Fax:
847-232-4042
Email:
info@newhopeinfusion.com
Treatments
Disclaimer
© 2024. All rights reserved.
Pages
Hours of Operation
Monday 9:00am- 5:00pm
Wednesday 9:00am- 5:00pm
If you or someone you care about is currently facing a crisis, we strongly urge you to contact the National Suicide Prevention Lifeline at 800-273-8255 or call 911 for immediate assistance.
